|
The Intensive Care Unit of most major hospitals is a noisy environment. In
order to monitor patients, healthcare practitioners set threshold alarms on
each of many individual vital sign monitors. While nurses themselves rarely
consider one vital sign in isolation, the current alarm algorithms elicit
numerous false positive alarms by only examining each vital sign individually.
The lack of clinical relevancy in a majority of these alarms produces an
inefficient healthcare system, where nurses habitually ignore low level alarms
due to their overabundance.
The Smart Alarms project consists of an alarm algorithm that considers
multiple vital signs when monitoring a post coronary artery bypass graft
(post-CABG) surgery patient. The nature of this condition enables the
algorithm to focus on monitoring four vital signs: blood pressure, heart rate,
respiration rate, and oxygen saturation rate. This solution constructs a new,
three level alarm priority system that more efficiently communicates the
clinical severity of the problem based on the needs and requests of current
healthcare practitioners. As a result, this multivariate approach decreases
clinical false alarms.
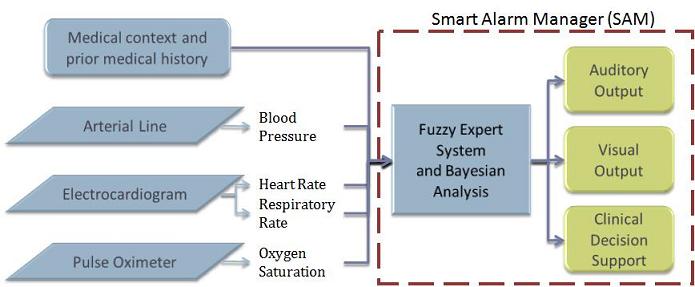
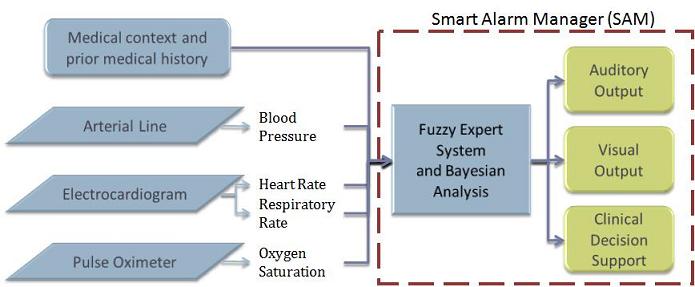
The algorithm takes the input of four vital signs from three monitors and
employs a Fuzzy Expert System to mimic the decision processes of nurses. In
addition, the algorithm includes a Clinical Decision Support tool that employs
Bayesian theory to display the possible CABG-related complications the patient
might be undergoing at any point in time, as well as the most relevant risk
factors.
Senior design project
Student team:
Ana R. Giannareas
Vanessa Kern
Nicholas Stevens
Adrian Viesca-Treviņo
|
Advisors:
Dr. Insup Lee
Dr. John Keenan
|
|
Domain expert:
Margaret Fortino-Mullen, MSN, RNGroup
|
Objectives
- Develop an alarm algorithm that considers multiple vital signs when
monitoring a post coronary artery bypass graft patient.
- Decrease the number of total alarms and of false alarms by vital sign
monitors by 25% without creating additional false negatives. For the purposes
of system validation in this project, false alarms are defined as those
resulting in no clinical intervention.
- Create a new, three level alarm priority system that more efficiently
communicates the clinical severity of the problem.
Why Coronary Artery Bypass Graft Surgery?
Attempting to reduce clinical alarms in all areas of patient care would be an
in-depth, several-years long endeavor. Our decision to focus on post-coronary
artery bypass graft (CABG) patients responded to:
- A need to narrow down our focus to a concrete clinical scenario.
- The well-researched nature of this procedure and its complications.
- The abundance of CABG surgeries in hospitals: 427,000 CABG surgeries
are performed every year in the United States.
System Diagram
Clinical Data Collection
System Design
The Smart Alarm Manager was designed with the input of 7 experienced nurses from the Univ. of Penn Health System.
Nurses provided data for the design of:
- Vital sign fuzzy sets
- Alarm levels for critical scenarios
- List of relevant complications, associated vital sign behavior and likelihood ratios
- Preferences for visual and auditory alarms
|
System Validation
Penn Presbyterian Medical Center (PMC)
The Smart Alarm Manager was tested using retrospective vital sign and contextual data from de-identified PMC SICU patients. The data was obtained with expedited IRB approval of Protocol #811401.
PhysioNet
The system was also tested with clinical data provided by PhysioNet.org, an MIT databank.
|
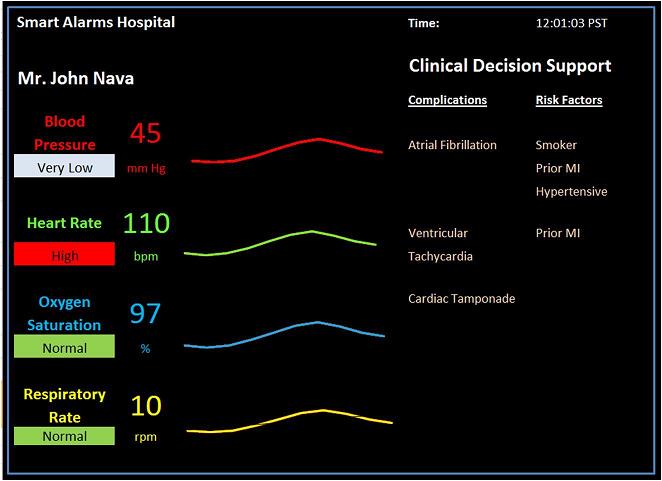
The Smart Alarm Monitor
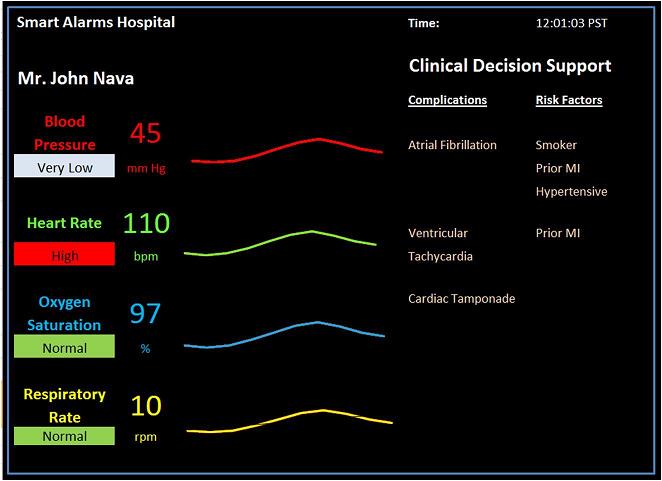
The Smart Alarm Monitor improves upon existing patient monitors by including color-coded alarm message boxes and by adding a clinical decision support tool that displays, in order of likelihood, the possible complications and the underlying risk factors present in the patient's medical history.
Results and Discussion
|
|
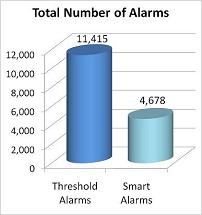
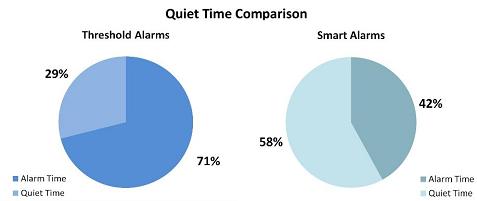
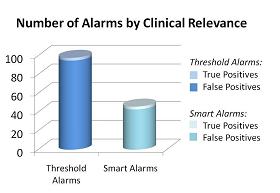
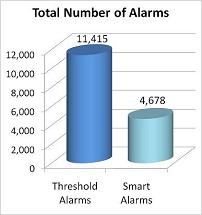
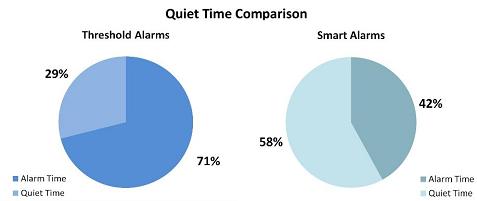
| Graphs 1 and 2: PhysioNet data (N=32 patients, 87061 min) |
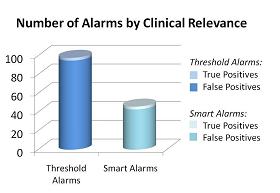
Graph 3: PMC data (N=5 patients, 7hrs)
|
Results from PhysioNet show:
- Number of alarms decreased by 59% (n=6737).
- Quiet time increased by 101% (n= 421 hrs).
Results from PMC show:
- Number of alarms decreased by 53% (n=52).
- False positives decreased by 55% (n=52).
- No change in false negatives, or missed alarms.
With a multivariate expert system, the Smart Alarm model succeeded in decreasing the number of false alarms.
|
|